Get More Time to Focus on Patients. Increase Cash Flow.
Our revenue-cycle management services remove the time-consuming processes that take you away from focusing on patient care and revenue-generating activities.

We Will Handle Billing and Collections. You Can Focus More Time on Your Patients.
Do you spend more time solving business tasks than you do helping patients? What if you could make your practice more efficient, increase your cash flow, and free up time to focus on your patients? Our billing and collections service can make that a reality.

Collect What You Earn
Rest easy in the assurance that we’ll submit your insurance claims, confirm their receipt, manage follow-ups and appeals, and verify timely, correct payment posting.
Enjoy Less Worry
Feel the weight lift off your shoulders as we verify accurate reimbursement, work up and send patient bills, follow up for payment, and handle the collections process.
Retain Real-Time Visibility
You’ll enjoy the ability to see AR reports and claim statuses anytime. Plus, you’ll have visibility into who your payers are.
Process Claims Quickly
As part of the onboarding process, electronic data interchange (EDI) is migrated or set up. Electronic funds transfer (EFT) is set up at this time as well.
Improve Patient Relations
You’ll earn credibility with your patients with timely, accurate statements and a patient portal for online payments. Plus, we act as advocates, questioning payers and ensuring they follow through on their promises.
Spend Less Time on Credentialing
Verifying to health insurers, hospitals, and surgery centers that you and your providers are qualified for patient care takes a lot of time. Let our team handle the credentialing, so your team can focus on practice operations.
Enjoy Faster Application Turnaround
Our credentialing services team has 15 years of experience, advanced credentialing software, and comprehensive knowledge of the processing requirements. Your applications are submitted without a hitch, every time, so there’s no delay in payment.
Reduce Busywork
Take the complex and time-consuming distraction of credentialing off your plate. We set up CAQH and then prepare, submit, and follow up on enrollment applications. We also track deadlines, expiration and renewal dates, and recredentialing requirements.
Devote Time to Priorities
Your current credentialing personnel can still serve as valuable Audigy resources. Without all the preparation, follow-up, and tracking tasks, however, they now have time to focus on process improvement, patient care, and driving revenue.

“I highly recommend Audigy for all of your credentialing needs and contract questions. I consider the small fees associated with what they do a bargain — more time back for me and my team to focus on the future!”
— Ashley Mitchell, First Coast Hearing Clinic

Manager of Coding and Contract Services
A Team to Simplify the World of Coding & Contracting

We will keep you up-to-date on regulatory changes that may impact your practice.

We can assist with contract renegotiations to ensure your practice is not negatively affected.
Get help understanding the third-party-payer landscape and how it could affect your practice.
Get answers to questions related to audiology billing and compliance.
“Audigy members are very fortunate to have Deb and her team as an in-house resource. They have provided me with invaluable insight and information to help me understand the hows and whys of filing claims that actually get paid.”
— Gina Trant, Hearing Healthcare, Practice Manager
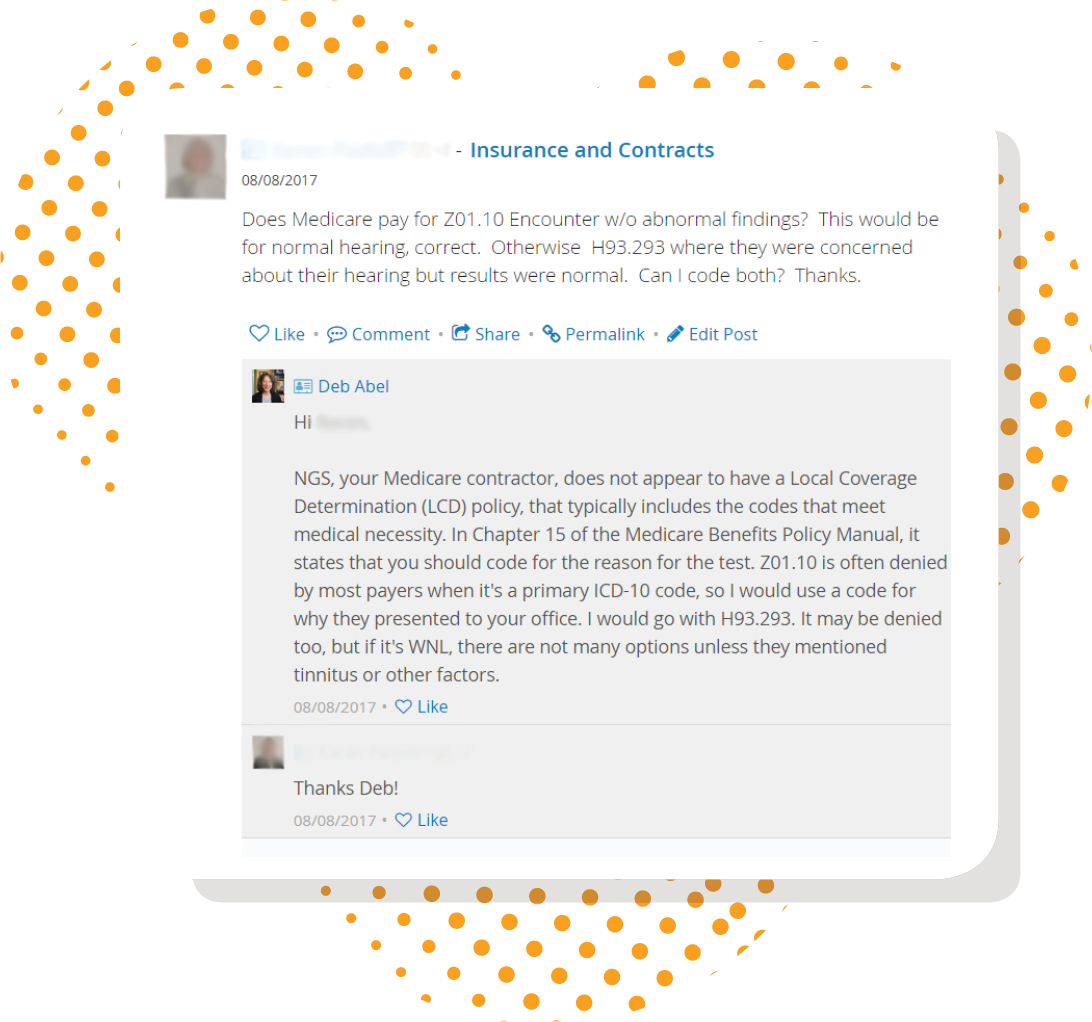
Get Billing and Coding Advice in a Live Forum
Audigy members get access to the live CEO Forum, where you can get billing and coding tips from owners, team members, and our billing and coding team.
See what other practices are asking regarding billing, coding, insurance, and third-party contracts.
Get answers to your questions from our billing and coding team.
Get feedback from practices across the country as to how they are handling certain insurance and contracting situations.